Euthanasia refers to the practice of intentionally ending a life in order to relieve pain and suffering. It is categorized as voluntary, non-voluntary and involuntary. Euthanasia can be further classified into active or passive ones. Active euthanasia is an intentional act to deliberately kill a terminally ill patient using various means whereas passive euthanasia happens when medical treatment is removed purposefully resulting in a person’s death to relieve him from unending pain. Until now euthanasia is not legalized in India.
Why in news-
- In 2016 Government proposed a draft bill on passive euthanasia for the first time called “The Medical Treatment of Terminally Ill Patients (Protection of Patients and Medical Practitioners) Bill”.
- Time and again widely debated across the media after the supreme court verdict on the Aruna Shanbaug case.
Aspirants would find this article very helpful while preparing for the UPSC 2022.
| Candidates can enhance their UPSC exam preparation by attempting UPSC Previous Years Question Papers now!!
To complement your preparation for the upcoming exam, check the following links: |
What is Euthanasia?
The phrase “euthanasia” was coined by Sir Francis Bacon. It is also called as ‘mercy killing’. The term “Euthanasia” has been derived from the two Greek words ‘eu’ and ‘thanotos’, which literally means ‘good death’.
Euthanasia is the practice of intentionally ending a life in order to relieve pain and suffering (provided motive should be good & death must be painless as much as possible) or
“A deliberate intervention was undertaken with the express intention of ending a life, to relieve intractable suffering.” – British House of Lords Select Committee on Medical Ethics.

| Difference between Euthanasia and physician-assisted suicide.
Physician-assisted suicide is often misunderstood with euthanasia. The difference being in who administers the lethal drug. In euthanasia-a physician or third party administers it. In physician-assisted suicide- it is the patient himself administers it, though on the advice of the doctor. Assisted suicide and euthanasia are sometimes called under the umbrella term “assisted dying”. |
Broad classification-
- Voluntary Euthanasia (with patients’ consent)– euthanasia is performed with the patients consent. It is legal in some countries like Belgium, Netherlands, etc.
- Non-voluntary Euthanasia (patient’s consent unavailable)– where a person is unable to give their consent (for example –the patient is in a state of coma or are severely brain-damaged) and another person takes the decision on their behalf, often because the ill person had expressed a wish previously to end their life in such circumstances.
- Involuntary Euthanasia (without asking consent or against the patient’s will)–Euthanasia conducted against the will of the patient is termed involuntary euthanasia. It is also regarded as murder.

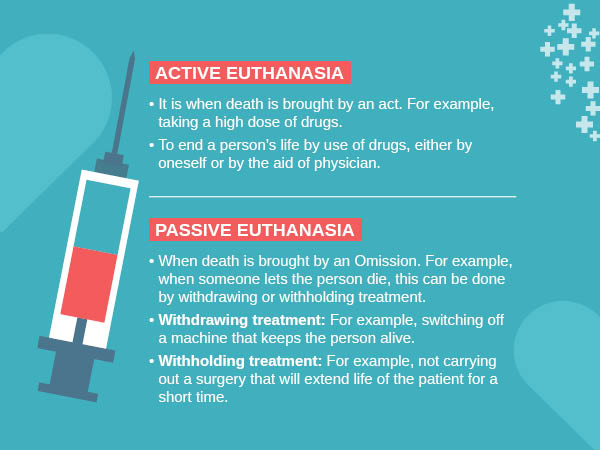
All types of euthanasia can be further divided into passive or active types-
a) Active Euthanasia– where a person intentionally intervenes to end someone’s life with the use of lethal substances or forces.
For example- Administering a lethal injection to end life.
b) Passive Euthanasia– where a person causes death by withholding or withdrawing treatment that is essential to maintain life.
For example- stoppage of antibiotics treatment in certain cases where it is necessary for the continuance of life, removal of life support system, etc
Debate- moral dilemma
Arguments For Euthanasia- According to euthanasia opponent Ezekiel Emanuel, proponents of euthanasia have presented four main arguments:
a) That people have a right to self-determination, and thus should be allowed to choose their own destiny.
b) Assisting a subject to die is a better option than continuing to suffer.
c) The distinction between passive euthanasia( which is frequently allowed) and active euthanasia is not substantive (the underlying principle–the doctrine of double effect is unreasonable) and
| The doctrine of double effect
The doctrine of double effect says that if doing something morally good has a morally bad side-effect, then it is ethically acceptable to do it provided the bad side-effect wasn’t intended. This is true even if you foresee that the bad effect would probably happen. The above principle is used to justify the case where a doctor gives drugs to a patient to lessen distressing symptoms in spite of knowing that doing so may shorten the patient’s life. This is because the doctor is not targeting directly to kill the patient, and the bad result of the patient’s death is a side-effect of the good result of reducing the patient’s pain. |
d) Allowing euthanasia will not necessarily lead to unacceptable consequences. Pro-euthanasia activists often take examples of countries like the Netherlands, Belgium, Luxembourg, etc. where euthanasia has been legalized to justify that it is mostly trouble-free.
Check the relevant links to prepare for the UPSC exam even better –
Other arguments-
Arguments based on rights
- People got an explicit right to die
- Death is a private subject and if there is no harm done to others then, the state and other people have no right to interfere (libertarian case)
Practical arguments–
- Death is a private subject and if there is no harm done to others then, the state and other people have no right to interfere (libertarian case)
- Allowing people to die may free up scarce health resources (this is a possible argument, but so far no authority has seriously proposed it)
Arguments Against Euthanasia
Similarly, Emanuel argues that there are four major arguments presented by opponents of euthanasia:
- All deaths are not painful.
- Termination of active treatment, combined with the effective use of pain relief are available as alternatives to euthanasia
- The distinction between active and passive euthanasia is morally significant and
- Legalizing euthanasia will put society on a slippery slope, which will lead to unacceptable consequences. (In Oregon 2013, the pain wasn’t one of the top five reasons that people sought euthanasia for. In fact, it was a loss of dignity, and a fear of burdening others).
Other arguments-
Ethical arguments
- Euthanasia could weaken society’s respect for the sanctity of life.
- Accepting euthanasia would mean that some lives (those of the sick or disabled) are worth less than others.
- Voluntary euthanasia could start on a slippery slope that may lead to involuntary euthanasia and the killing of people who are thought undesirable.
- Euthanasia might not be in a person’s best interests.
- Euthanasia affects the rights of other people and not just those of the patient
Religious arguments- Religions are opposed to euthanasia for a number of reasons.
a) Euthanasia is against the will and word of God. (God has forbidden it)
- Virtually all religions in their scriptures say ‘you must not kill’. Therefore carrying out any of these would be against God’s command, and would be an attack on the sovereignty of God
b) Euthanasia weakens society’s respect for the sanctity of life.
- Human life is sacred. Human lives are special because God created them. Human beings are made in God’s image. Therefore human life should be protected and preserved, whatever happens
c) law of karma –Suffering may have value (Freedom from worldly life)
- Hinduism and Buddhism see mortal life as part of a continuing cycle in which we take birth, live, die, and are reborn over and over again.
- During each cycle of life and death, human beings make progress towards their ultimate aim, which is liberation.
- Thus, shortening life interferes with the law of karma.
d) Voluntary euthanasia could start on a slippery slope that may lead to involuntary euthanasia and the killing of people who are thought undesirable
e) Most religions disapprove of euthanasia. Some absolutely forbid it.
For example, the Roman Catholic church is one of the most active organizations in opposing euthanasia.
f) Virtually all religions state that those who become vulnerable through illness or disability deserve special care and protection, and proper care of life is a much better thing than euthanasia.
g) Non-harm – the principle of ahimsa-Hinduism and Buddhism regard all life as precious. (not just human life). They say that we should try to avoid harming living things and therefore this also rules out killing people, even if they want to die.
Practical arguments
- Proper palliative care could make euthanasia unnecessary.
- Euthanasia cannot be properly regulated
- Permitting euthanasia will lead to less good care for the terminally ill.
- Permitting euthanasia could undermine the commitment of doctors and nurses to save lives.
- Euthanasia may become in the future a cost-effective way to treat the terminally ill.
- Allowing euthanasia could discourage the search for new modes of treatment for the terminally ill.
- Euthanasia could discourage the motivation to provide good care for the dying.
- Euthanasia gives too much authority to doctors.
- Euthanasia exposes vulnerable people to pressure to end their lives.
- Moral pressure on elderly people by selfish families.
- Moral pressure to free up medical resources.
- Patients may feel euthanasia is the only way out when they are abandoned by their families.

Indian scenario
| India’s Euthanasia Timeline
In the Gyan Kaur case, the Supreme Court held that both euthanasia and assisted suicide are not lawful in India. The Court confusingly stated- 1) The right to life under Article 21 of the Constitution does not include the right to die. The court held that Article 21 is a provision guaranteeing protection of life and personal liberty and by no stretch of imagination can extinction of life be read into it. 2) The right to live with dignity does include the right to die with dignity But the court could not come up with any practical rules and passed the buck to lawmakers to come up with laws regulating euthanasia In 2006, the 196th report of the Law Commission of India brought out `The Medical Treatment of Terminally ill Patients (Protection of Patients and Medical Practitioners) Bill 2006. However, no law was made on euthanasia. In 2011 the supreme court in Aruna Shanbaug versus Union of India case laid down guidelines to process pleas for passive euthanasia. It said till Parliament works out legislation, the procedures laid down by the guidelines should be followed. It also spelled out differences between active and passive euthanasia. In 2012, The Law Commissions 241st report again proposed making legislation on passive euthanasia and prepared a draft bill called the Medical Treatment of Terminally Ill Patients (protection of patients and medical practitioners) Bill. Bill deals with passive euthanasia and living will. It doesn’t recommend active euthanasia In 2014, a three-judge bench of the Supreme Court of India had called the judgment in the Aruna Shanbaug case to be ‘inconsistent in itself’ and has referred the subject of euthanasia to its five-judge Constitution bench. In 2016, the Health ministry uploads the draft bill for public opinion -The Medical Treatment of Terminally Ill Patients (Protection of Patients and Medical Practitioners) Bill and wants people to give their views so that it can take a decision to enact/not to enact a law on passive euthanasia. |
| Supreme Court guidelines on passive euthanasia
The following guidelines were laid down for carrying out passive euthanasia. 1. The decision to discontinue life support needs to be taken either by the parents or the spouse or other close relatives or in the absence of any of them, such a decision can be taken even by a person or a body of persons acting as a next friend. 2. Such a decision can also be taken by the doctors attending the patient as bonafide in the best interest of the patient. 3. Every such decision needs approval from the concerned High Court. 4. When a high court receives such an application, the Chief Justice should constitute a Bench of at least two Judges who should decide to grant approval or not. This bench will nominate and need a report from a committee of three reputed doctors. 5. Before giving the verdict a notice regarding the report should be given to the close relatives and the State. After hearing the parties, the High Court can give its verdict. |
The Medical Treatment of Terminally Ill Patients (Protection of Patients and Medical Practitioners) Bill
Key terms-
- Advance medical directive- also called a living will. It means a directive given by a person that he/she as the case may be shall or shall not be given medical treatment in the future when he/she becomes terminally ill.
- Palliative care–
a) Provision of reasonable medical and nursing procedures for relief of physical pain, suffering, discomfort, or emotional or psychosocial suffering.
b) A reasonable provision for food and water.
- Competent patient– a patient who is not an incompetent patient.
- Incompetent patient- means a minor who is below 16 years of age or of unsound mind or a patient who is unable to-
a) understand information relevant to an informed decision about his/her medical treatment.
b) Retain and use that information to make decisions
c) Not able to make an informed decision due to disturbance in the functioning of the brain/mind.
d) Communicate his /her informed decision by speech, sign, language, or any other mode.
- Informed decision- means the decision as to continuance or withholding or withdrawing medical treatment taken by a patient who is competent and who is or has been informed about-
a) The nature of his/her illness
b) Any alternative form of treatment that is available
c) The consequences of those forms of treatment and
d) Consequences of remaining untreated
- Terminal illness-such illness/injury/degeneration of physical or mental condition which is causing extreme pain and suffering to the patients and according to the medical opinion will inevitably cause the untimely death of the patient concerned
Or
Meaningful existence of life is not possible due to irreversible vegetative condition.
Salient Provisions of the Draft Bill
- Every competent patient, including minors aged above 16 years, has a right to make a decision and express their desire to the medical practitioner attending on her or him on whether to continue further treatment or allow nature to take its own course.
- The Bill provides protection to patients and doctors from any liability for withholding or withdrawing medical treatment and states that palliative care (pain management) can continue.
- When a patient communicates her or his decision to the medical practitioner, such a decision is binding on the medical practitioner. However, it also notes that the medical practitioner must be “satisfied” that the patient is “competent” and that the decision has been taken on free will.
- There will be a panel of medical experts to decide on a case by case basis.
- The medical practitioner has to maintain all details of the patient and ensure he/she takes an informed decision. He is also required to inform the patient whether it would be best to withdraw or continue treatment. If the patient is not in a conscious state, he/she needs to inform family members. In the absence of family members, the medical practitioner needs to inform a person who is a regular visitor.
- The draft also lays down the process for seeking euthanasia, right from the composition of the medical team to move the high court for permission.
- Permission to be obtained from the high court. Any near relative, friend, legal guardian, medical doctor/staff attending the patient, any other person obtaining the leave of the court can apply to the jurisdictional high court. Such an application is treated as an original petition and the chief justice of the high court shall assign the same to the divisional bench without loss of time and the same should be disposed of as far as practical within a month. This bench will nominate and need a report from a committee of three reputed doctors.
- The Bill only portends to legalize what is called “passive euthanasia”, as discussed in the judgement pertaining to Aruna Shaunbaug. Active euthanasia is not being considered “as it is likely to be used by unscrupulous individuals to attain their ulterior motives.”
- Advanced medical directive or living will be void and not binding on any medical practitioner.
- The medical council of India may issue guidelines consistent with the provisions of the bill. It may review and can also modify from time to time
Probable concerns- There have been mixed reactions to the draft bill. Some consider it a “good start”, but others didn’t quite agree. Some of the probable concerns are-
- The draft has disappointed experts who wanted complete clarity on the concept of a living will. While there have been demands for recognizing Advance Medical Directives (also known as a living will) whereby a person declares in advance whether or not treatment should be given if he is terminally-ill and incompetent to take decisions in the future, the government has rightly shot down the proposal.
- Child rights activists opine that in India, signing a contract or marrying before the age of 18 is not permitted, then how can a child decide to live or die.
- concerns for its misuse remain a major issue which ought to be addressed before it becomes a law in our country-
a) Doctors may come under the influence of corruption and fabricate material to prove that it is a terminal case with no chance of recovery.
b) Leaving it solely to the patient’s relatives or to the doctors or next friend to decide whether to withdraw the life support of an incompetent person, there is always a risk that this may be misused by some unscrupulous persons who wish to inherit or otherwise grab the property of the patient.
What is a “living will” and what are debates and arguments in relation to a living will?
In 2014, the Supreme Court had issued notice to all the states seeking their views on whether a terminally ill person can execute a “living will” that his or her life support system be withdrawn if he or she reaches a vegetative state with no hope of revival. The court has also appointed amicus curiae.

A Living Will is a document that sets out a patient’s wishes regarding health care and how they want to be treated if they become seriously ill and unable to make or communicate their own choices. Living wills are also called as active declarations.
Arguments For living will-
- They respect the patient’s human rights, and in particular their right to reject medical treatment.
- Creating them encourages full discussion about end of life decisions.
- Knowing what the patient want means that doctors are more likely to give appropriate treatment.
- They help medical professionals in taking difficult decisions.
- A patient’s family and friends don’t have to take the difficult decisions
Arguments against a living will-
- Writing them may be very depressing.
- It’s difficult for a healthy person adequately to imagine what they would really want in the situations where a living will take effect.
- It may be hard to translate the words of the living will into actual medical action.
- Patients may change their minds but not change their living wills.
- They’re no use if they can’t be found quickly when needed.
In India attempt to commit suicides (Section 309 of the Indian Penal Code ) and abetment of suicide( Section 306 of the IPC) are crimes and both actions are punishable. The problem is that to be able to make a living will, the legislation would need to decriminalize both. Though the court should consider the legitimacy of a will, there are several issues. For example, if the death of the patient is of material value to those are who close to him/her (such as property), the suspicion over the validity of the living can become a legal issue. Thus, there is a need to carefully set up conditions under which a living will be executed.
Summary- There is no point in prolonging the physical agony of a terminally ill person and the mental trauma of their loved ones. Therefore, euthanasia should be made legal in cases where there is no scope of a patient recovering. India however requires a mix of sensitivity and maturity for such an important decision to be taken as it involves ‘right to life’ and ‘right to die with dignity’.
“He who has health has hope, and he who has hope has everything”.-Arabic Proverb
How to approach for the Civil Services Examination
Essay-
Death is a private matter and if there is no harm to others, the state has no right to interfere.
Human life is sacred. Irrespective of the pain and suffering, human life should be protected and preserved.
GS Paper II- Health-related aspect (public health and safety. Welfare etc)
Practice Questions –
In Prelims-
Which of the following statement is /are correct
- Article 21 of the constitution also deals with the right to die.
- The draft bill legalizes active euthanasia in India.
- According to the draft bill on passive euthanasia, the advanced medical directive shall be void and not binding on any medical practitioner.
- The draft Bill also provides for active euthanasia and physician-assisted suicide in certain cases.
In Mains-
GS paper II-
- Is passive euthanasia finally going to be a reality in India? Discuss?
- Critics of euthanasia claim that Voluntary euthanasia is the start of a slippery slope that leads to involuntary euthanasia and the killing of people who are considered undesirable. Critically discuss?
- Allowing euthanasia undermines the commitment of doctors and nurses to save lives. Critically discuss?
FAQ about Euthanasia or Mercy Killing
Is euthanasia legal in India?
What are the different types of euthanasia?
UPSC exam related links are given below for candidates convenience in the preparation.
Comments